3M Bair Hugger temperature management solutions
Science of warming: Normothermia management from start to finish
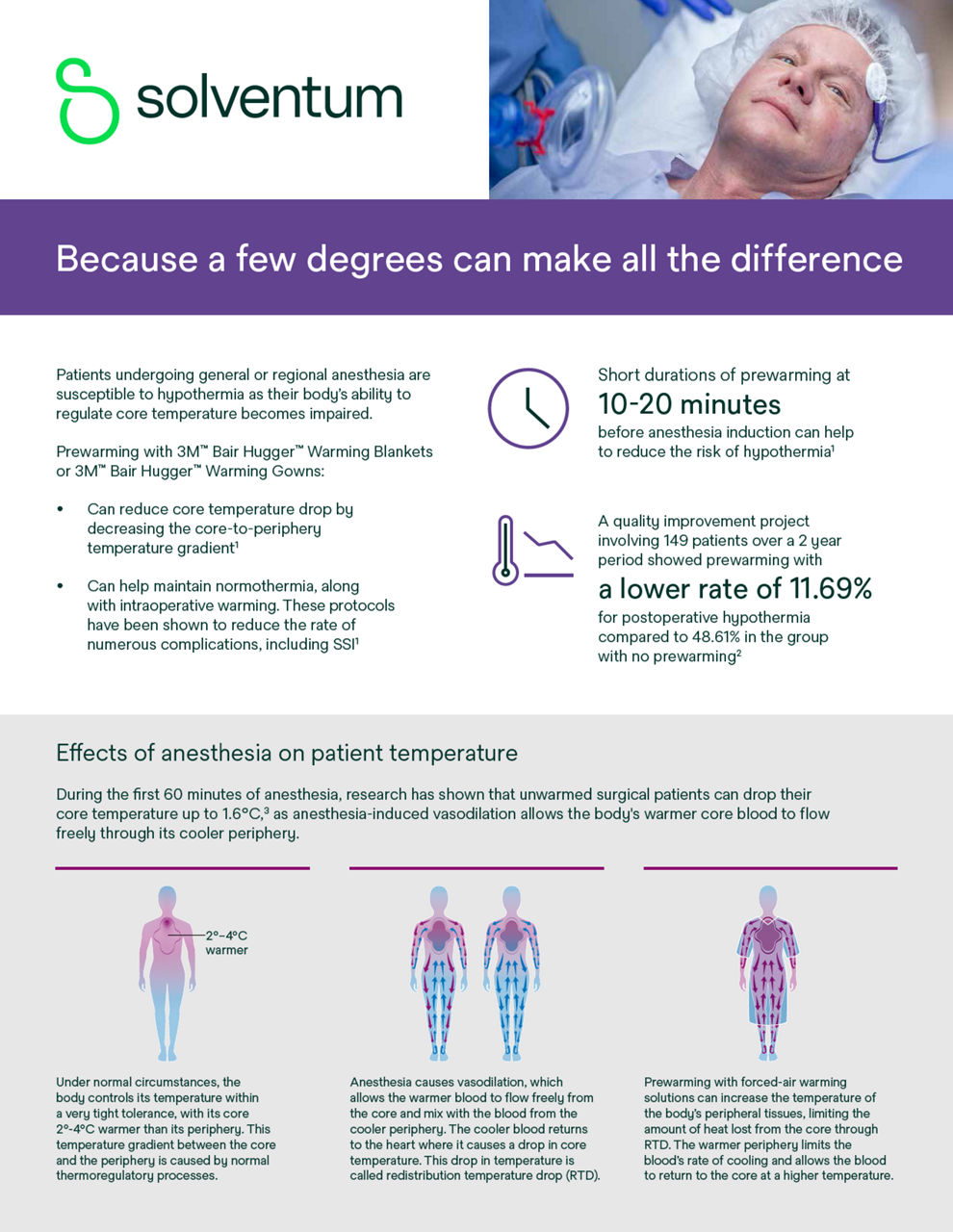
The difference between a successful patient outcome and a complicated recovery can often be determined by a few degrees difference in body temperature. Unintended perioperative hypothermia is a common yet avoidable complication of anesthesia, known to increase the risk of surgical site infection (SSI),6,7 prolong recovery time,8 and even elevate mortality rates.9 However, by following a normothermia protocol which includes vigilant temperature monitoring and proactive warming measures prior to anesthesia induction through to recovery, hypothermia can be preventable.
Start and end your patients’ perioperative journey with our 3M Bair Hugger Temperature Management System
By maintaining a normothermic core body temperature a patient's length of stay can be reduced by 2.6 days.11
How to proactively manage normothermia throughout the perioperative journey:
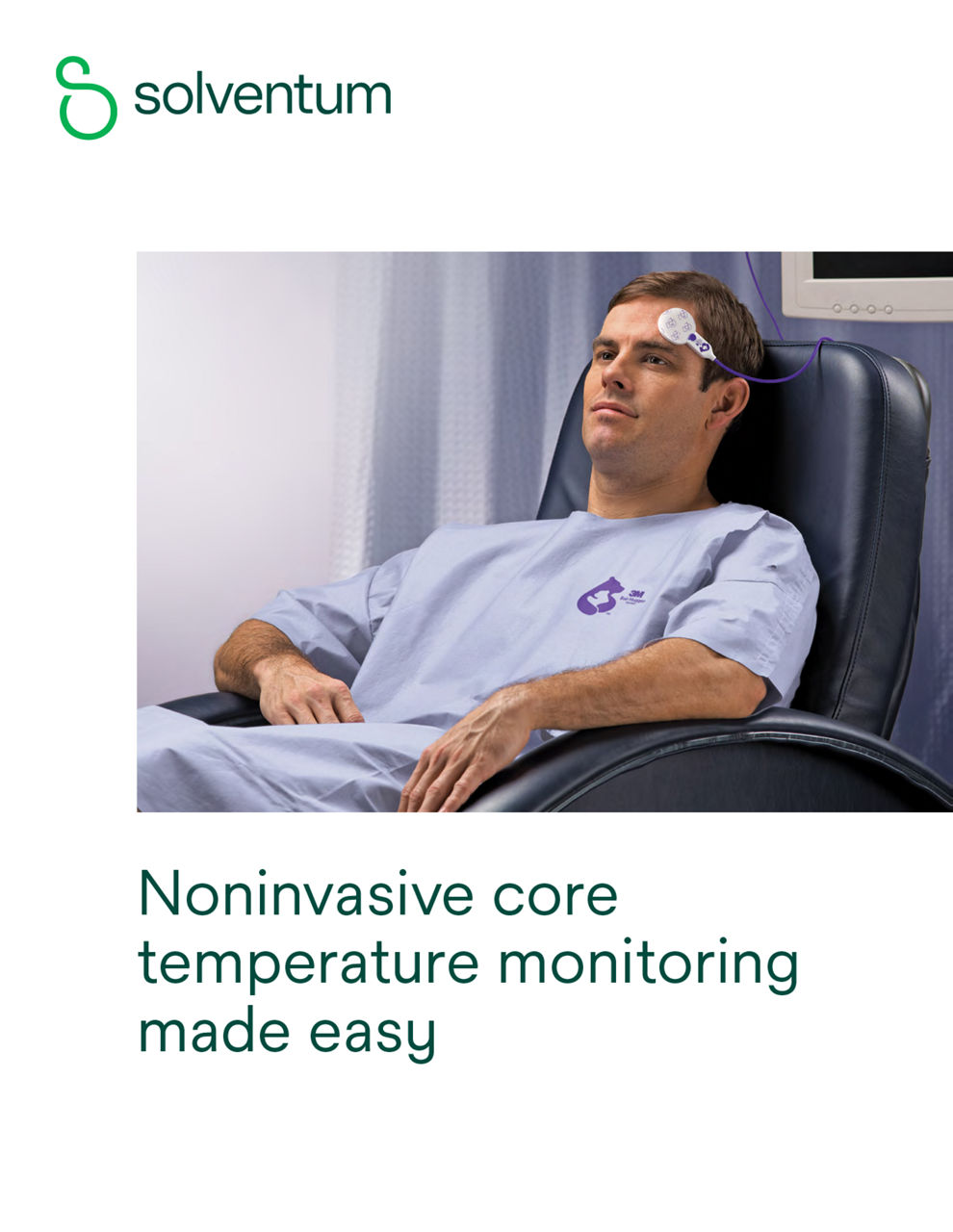
Actively measure your patients’ temperature. Prewarm them with the 3Mᵀᴹ Bair Huggerᵀᴹ Warming System to help prevent hypothermia.
Preoperative (pre-op)
Prewarming prior to the induction of anesthesia helps to maintain normothermia and mitigate the effects of heat redistribution caused by anesthesia.
Monitor your patients’ core body temperature during surgery with the 3Mᵀᴹ Bair Huggerᵀᴹ Temperature Monitoring System. Proactively help achieve and maintain normothermia with 3Mᵀᴹ Bair Huggerᵀᴹ Warming System.
Intraoperative (intra-op)
Continue to monitor your patients’ temperature. Warm them with our 3Mᵀᴹ Bair Huggerᵀᴹ Warming System to help protect patients from unintended perioperative hypothermia.
Postoperative (post-op)
By maintaining a patient’s core body temperature near 36.5°C (36.6 + or - 0.5°C), patient length of stay has been shown to be reduced by 2.6 days.21
3M Bair Hugger temperature management solutions
NOTE: Specific indications, limitations, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
Resources to help maintain normothermia
The temperature monitoring process can be overwhelming. We offer useful resources to help you learn more about our solutions and how they can help you monitor and maintain your patients’ normal core body temperature — normothermia — throughout their perioperative journey.
References:
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209-1215.
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209-1215.
- Bush HL Jr, Hydo LJ, et al. Hypothermia during elective abdominal aortic aneurysm repair: the high price of avoidable morbidity. J Vasc Surg. 1995;21:392-400; discussion 400-392.
- Lau A, Lowlaavar N, Cooke EM, et al. Effect of preoperative warming on intraoperative hypothermia: a randomized-controlled trial. Can J Anesth. 2018. doi.org/10.1007/s12630-018-1161-8.
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. NEJM. 1996 May 9; 334 (19): 1209-16.
- Horn, EP, Bein B, Bohm R, Steinfath M, Sahilin, and Hocker J. The effect of short time periods of pre-operative warming in the prevention of peri-operative hypothermia. Anaesthesia. 2012; 67: 612–617.
- Nelson G, Altman AD, Nick A, et al. Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations — Part I. Gynecologic Oncology. 2015; 2016; 140: 313-322.
- National Institute for Health and Care Excellence. Hypothermia: prevention and management in adults having surgery. Clinical Guideline [CG65]. (2016). https://www.nice.org.uk/guidance/cg65/chapter/Recommendations#perioperative-care. Published April 2008. Updated December 2016. Accessed July 18, 2019.
- Forstot RM. The etiology and management of inadvertent perioperative hypothermia. J Clin Anesth. 1995;7:657-674.
- Leslie K, Sessler DI. Perioperative hypothermia in the high-risk surgical patient. Best Pract Res Clin Anaesthesiol. 2003;17:485-498.
- Mahoney CB, Odom J. Maintaining intra-operative normothermia: a meta-analysis of outcomes with costs. AANA J. 1999;67(2):155-163.
- Schroeck H, Lyden AK, Benedict WL, Ramachandran SK. Time Trends and Predictors of Abnormal Postoperative Body Temperature in Infants Transported to the Intensive Care Unit. Anesthesiology Research and practice. 2016:7318137.
- Hooper VD, Chard R, Clifford T, Fetzer S, Fossum S, Godden B, Martinez EA, Noble KA, O’Brien D, Odom-Forren J, Peterson C, Ross J, Wilson L. ASPAN’s Evidence-Based Clinical Practice Guideline for the Promotion of Perioperative Normothermia: Second Edition. J PeriAnesth Nurs. Vol 25, No 6 (December), 2010: pp 346-365.
- 3M Data on File: EM-05-297733, EM-05-711315.
- 3M™ Bair Hugger™ System Research Compendium, 2017 at: FAWFACTS.com.
- 3M Data on File: EM-05-233213, EM-05-268428.
- U.S. News and World Report. America’s Best Hospitals: the 2023-2023 Honor Roll and Overview. U.S. News and World Report website. Accessed December 2023 .https://health. usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview.
- Horn, EP, Bein B, Bohm R, Steinfath M, Sahilin, and Hocker J. The effect of short time periods of pre-operative warming in the prevention of peri-operative hypothermia. Anaesthesia. 2012; 67: 612–617.
- Lau A, Lowlaavar N, Cooke EM, et al. Effect of preoperative warming on intraoperative hypothermia: a randomized-controlled trial. Can J Anesth. 2018. doi.org/10.1007/s12630-018-1161-8.
- National Institute for Health and Care Excellence. Hypothermia: prevention and management in adults having surgery. Clinical Guideline [CG65]. (2016). https://www.nice.org.uk/guidance/cg65/chapter/Recommendations#perioperative-care. Published April 2008. Updated December 2016. Accessed July 18, 2019.
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. NEJM. 1996 May 9; 334 (19): 1209-16.
- Horowitz PE, Delagarza MA, Pulaski JJ, Smith RA. Flow rates and warming efficacy with Hotline and Ranger blood/fluid warmers. Anesth Analg. 2004; 99 (3): 788-792.
- Nelson G, Altman AD, Nick A, et al. Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations — Part I. Gynecologic Oncology. 2015; 2016; 140: 313-322.
- Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA. 1997; 277 (14): 1127-1134.
- Scott AV, Stonemetz JL, Wasey JO, Johnson DJ, Rivers RJ, Koch CG, et al. (2015) Compliance with Surgical Care Improvement Project for Body Temperature Management (SCIP Inf-10) Is Associated with Improved Clinical Outcomes. Anesthesiology. 123: 116–125.
- Anderson DJ. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infection Control and Hospital Epidemiology. 2014; 35 (6): 605–627. doi: 10.1086/676022. Accessed December 15, 2016.
- Melling AC, Ali B, Scott EM, Leaper DJ. Effects of preoperative warming on the incidence of wound infection after a clean surgery: a randomized controlled trial. Lancet. 2001; 358 (9285): 876-880.
- Van Duren A. Patient Warming Plays a Significant Role in Satisfaction, Clinical Outcomes. Infection Control Today. 2008; 12 (6): 1-4 (reprint page numbers).
- Rajagopalan S, et al. The Effects of Mild Perioperative Hypothermia on Blood Loss and Transfusion Requirement. Anesthesiology. 2008; 108: 71-7.