Venous leg ulcer (VLU)
Tackling VLU one step at a time
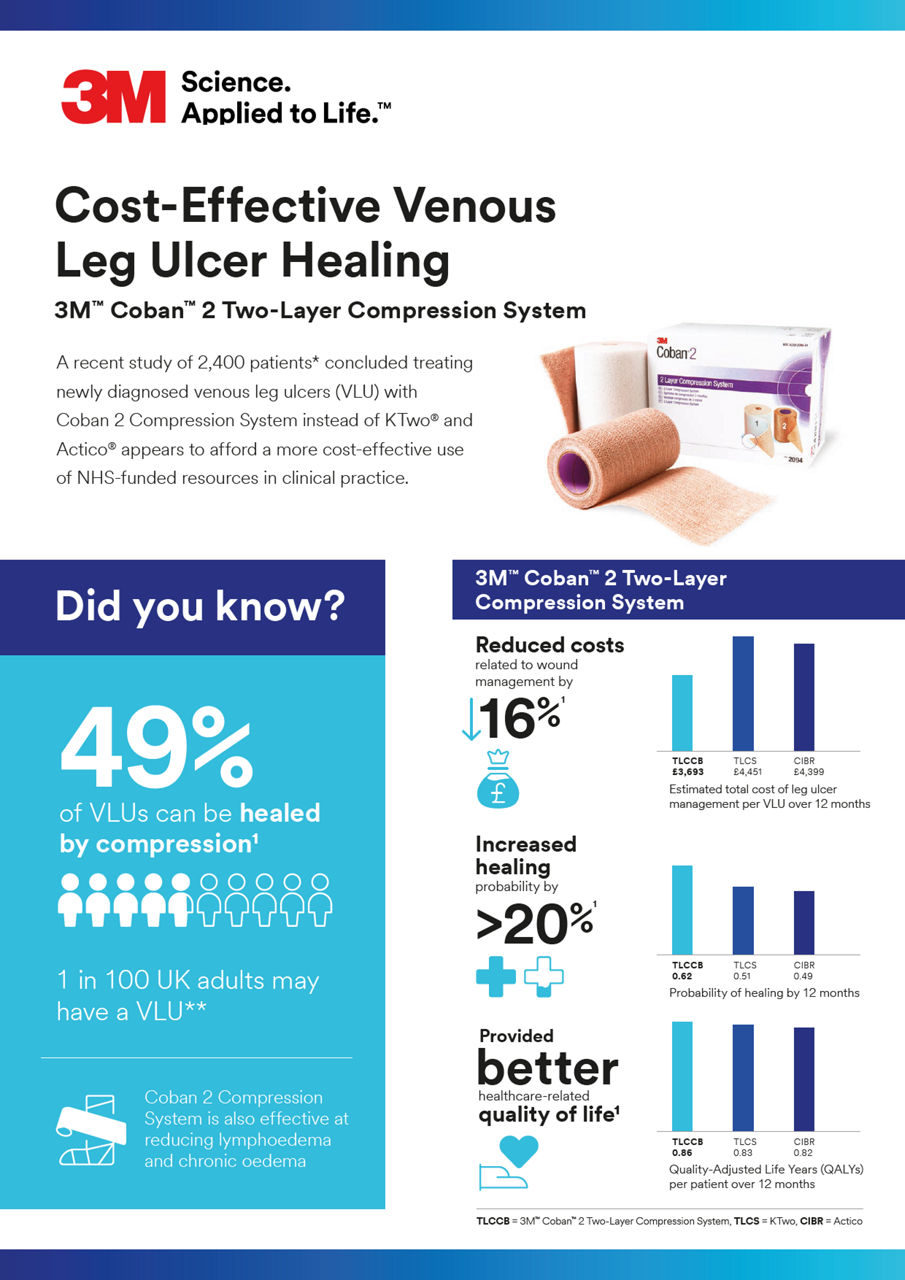
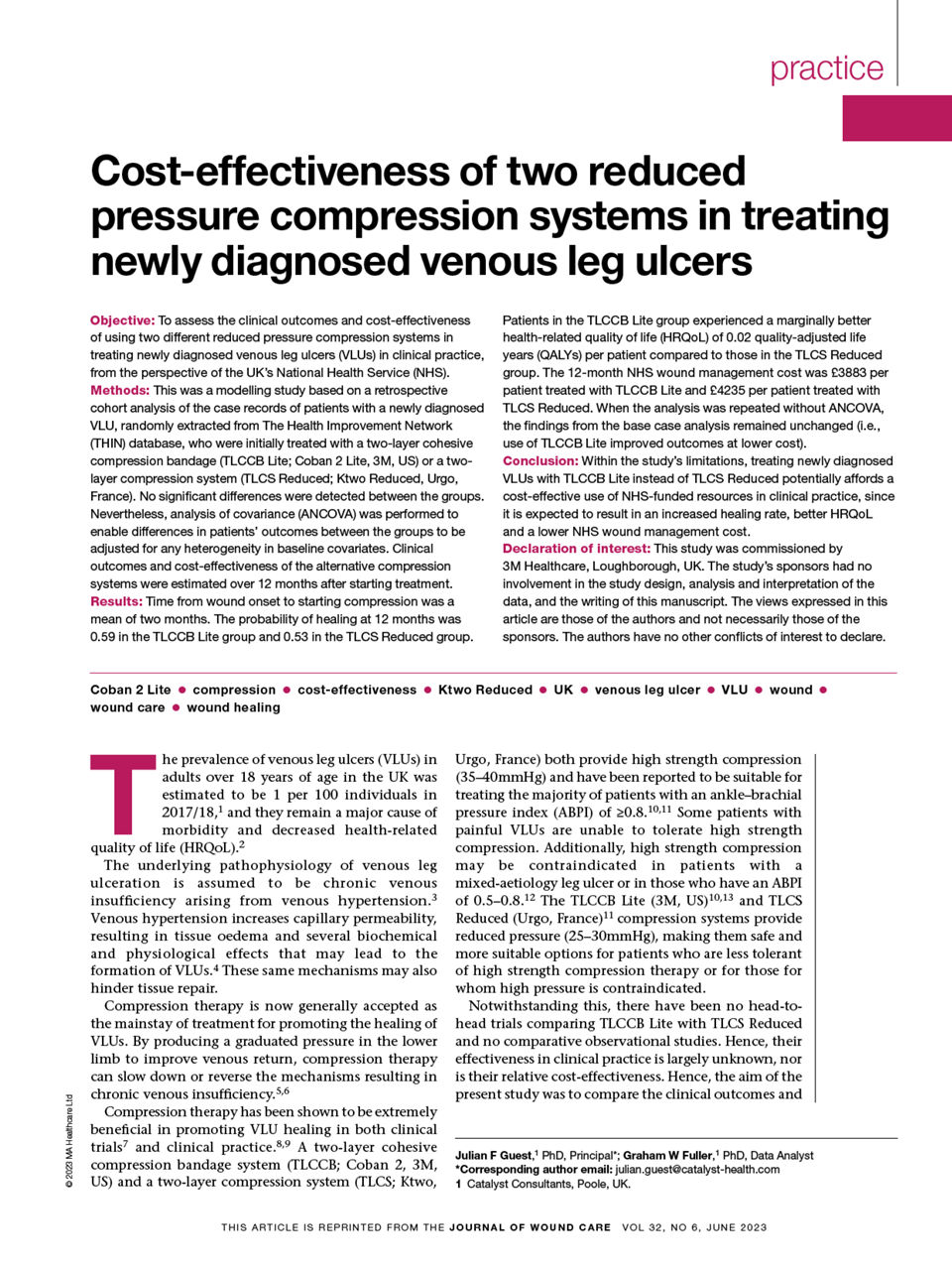
Venous leg ulcers (VLU) present a major challenge for patients and clinicians around the world. In fact, it is the most common type of lower extremity wound affecting approximately 1% of the western population during their lifetime¹, not only causing significant pain and discomfort for patients, but also presenting significant financial burdens for them and healthcare systems.²
We understand the challenges associated with VLUs. Our clinically proven solutions are designed to promote wound healing, help patients regain their mobility, and empower them to live to their fullest.
Three easy steps to help you simplify VLU management
Managing venous leg ulcers involves combining clinical best practices and wound care principles with the goal of reducing chronic oedema and promoting healing.⁶⁻⁸ According to an article published by Wounds International in 2015, the consensus breaks down the assessment and management of venous leg ulcers into three main steps, known as the ABC model of care.⁶
Follow these steps to provide effective care and help your patients on their healing journey:
Solutions designed with comfort and mobility in mind
Wound management systems have direct impact on a patient’s healing journey and quality of life.
From dressings that manage exudate and protect against bacterial contamination to skin care products that empower skin health, you can promote effective recovery with solutions that support healing, provide comfort, and help patients return to their daily lives.
Explore our solutions below and find the right product for your patient’s needs.
Negative pressure wound therapy (NPWT) portfolio
Every wound has its unique healing. We offer you a comprehensive range of proven NPWT solutions, designed to treat a wide a variety of wounds, including venous insufficiency, enabling you to improve wound care and outcomes.
In fact, NPWT has been shown to be effective for patients with VLU wounds that have been present for more than 30 days.¹³* Explore our proven solutions below.
Traditional NPWT
The ActiV.A.C. Therapy System is a portable NPWT device for the mobile patient designed to help maintain the prescribed pressure at the wound site and detect leaks.
V.A.C.® Therapy can help to reduce hospitalisation time and the risk of complication, facilitating patient transitions from inpatient to outpatient care settings.
Veraflo Therapy combines the benefits of V.A.C.® Therapy with automated instillation and dwell of topical wound solution to provide simultaneous cleansing and granulation tissue formation.
The Veraflo Cleanse Choice Dressing features three foam layers to provide application options for wounds with varying depths and allows for single or duo pad application.
Single-use NPWT
The Snap Therapy System is a disposable NPWT system that combines the simplicity of advanced wound dressings with the proven benefits of negative pressure wound therapy in a discreet design and allows patient mobility.
Discover how you can deliver quality care more easily and safely for your patients. Connect with us to request a demo or learn more about our products.
*NPWT is not indicated for use with compression.
Real patients, real results

The problem
An 86-year-old woman presented to the clinic for management of a trauma injury measuring over 20cm in length to the lateral right leg following a fall. Previous medical history included anaemia and hypertension. Previous treatment included various dressings, which did aid healing but did not address the underlying disease. A full assessment of the leg and ulcer indicated clear evidence of venous disease with hemosiderin staining and underlying oedema.14
The solution
The ulcer required exudate management and the limb required oedema reduction. The wound was cleansed, and emollients were applied to improve the surrounding skin. 3M™ Kerramax Care™ Super-Absorbent Dressing was applied to manage the exudate and the 3M™ Coban™ 2 Two-Layer Compression System to reduce the oedema. After 2 weeks, the exudate and oedema were sufficiently reduced; the dressing regimen was changed to a non-adherent dressing. The Coban 2 Layer Compression System was continued. The wound was almost healed at 12 weeks. At that point the compression system was discontinued, and a 2-layer hosiery kit was implemented with a foam dressing. The wound progressed to complete healing after 15 weeks.14
The patient reported that combination of the Kerramax Care Dressing and Coban 2 Layer Compression System was very comfortable; the low profile allowed her to continue wearing her usual footwear. The compression system did not slip during wear and was easy to remove at the weekly check-up visits. The recommended long-term management plan would be to wear compression hosiery; however, this patient declined. She did agree to continue to moisturise her skin with emollients to reduce the risk of skin breakdown.14
Review more case studies
Helpful resources for you and your patients
3M™ Coban™ Two-Layer Compression System appliance
How to apply and remove compression systems
Download our comprehensive resource guides for step-by-step instructions on how to apply our Coban 2 Compression System. These guides will help you confidently deliver effective compression therapy and enhance your patient’s experience.
Support resources
- Simka, Marian, and Eugeniusz Majewski. "The social and economic burden of venous leg ulcers: focus on the role of micronized purified flavonoid fraction adjuvant therapy." American journal of clinical dermatology 4, no. 8 (2003): 573-581.
- Brem, Harold, Robert S. Kirsner, and Vincent Falanga. "Protocol for the successful treatment of venous ulcers." The American Journal of Surgery 188, no. 1 (2004): 1-8.
- Rice, J. Bradford, Urvi Desai, Alice Kate G. Cummings, Howard G. Birnbaum, Michelle Skornicki, and Nathan Parsons. "Burden of venous leg ulcers in the United States." Journal of medical economics 17, no. 5 (2014): 347-356.
- Finlayson, Kathleen J., Christina N. Parker, Charne Miller, Michelle Gibb, Suzanne Kapp, Rajna Ogrin, Jacinta Anderson, Kerrie Coleman, Dianne Smith, and Helen E. Edwards. "Predicting the likelihood of venous leg ulcer recurrence: the diagnostic accuracy of a newly developed risk assessment tool." International wound journal 15, no. 5 (2018): 686-694.
- Weller C, Buchbinder R, Johnston R. Interventions for helping people adhere to compression treatments for venous leg ulceration (Review). Cochrane Database Syst Rev. 2013;9.
- Harding K. et al. Simplifying venous leg ulcer management. Consensus recommendations. Wounds International. 2015;10–11.
- O’Donnell Jr, Thomas F., Marc A. Passman, William A. Marston, William J. Ennis, Michael Dalsing, Robert L. Kistner, Fedor Lurie et al. "Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery® and the American Venous Forum." Journal of vascular surgery 60, no. 2 (2014): 3S-59S.
- Kelechi, Teresa J., Glenda Brunette, Phyllis A. Bonham, Lea Crestodina, Linda R. Droste, Catherine R. Ratliff, and Myra F. Varnado. "2019 guideline for management of wounds in patients with lower-extremity venous disease (LEVD): An executive summary." Journal of Wound Ostomy & Continence Nursing 47, no. 2 (2020): 97-11.
- Partsch, H., and P. Mortimer. "Compression for leg wounds." British Journal of Dermatology 173, no. 2 (2015): 359-369.
- Partsch, H., and C. Moffatt. "An overview of the science behind compression bandaging for lymphoedema and chronic oedema." Compression Therapy: A position document on compression bandaging. International Lymphoedema Framework in association with the World Alliance for Wound and Lymphoedema Care (2012): 12-22.
- Moffatt, Christine, H. Partsch, J. Schuren, I. Quéré, M. Sneddon, M. Flour, A. Towers et al. "Compression therapy: a position document on compression bandaging." Int Lymph Fram J (2012): 12-23.
- Mosti, G. "Venous ulcer treatment requires inelastic compression." Phlebologie 47, no. 01 (2018): 7-12.
- Marston, William A., David G. Armstrong, Alexander M. Reyzelman, and Robert S. Kirsner. "A multicenter randomized controlled trial comparing treatment of venous leg ulcers using mechanically versus electrically powered negative pressure wound therapy." Advances in wound care 4, no. 2 (2015): 75-82.
- STUD, ASE, and Y. SERIES. "3M™ Kerramax Care™ Super-Absorbent Dressing and 3M™ Coban™ 2 Two-Layer Compression System." (2022).